Alternative Provider IDs in REF02
An explanation of how to handle alternate ID submission for specific insurance carriers in AngelTrack
Some insurance carriers require an alternate ID to be sent in loop 2310B element REF02, also known as "CMS-1500 box 24j". AngelTrack supports this request.
Configuring Your Alternate IDs
If you must submit an alternate ID number with your insurance claims in loop 2310B (rendering provider) or in loops 2010AA (billing provider) or 2010BB (primary insurance payor ID), then you must input these alternate IDs into AngelTrack. This is done using the Billing Configuration page under Settings. Each alternate ID must include:
- Alternate ID qualifier (REF01), which is usually "G2" (carrier-assigned ID number) but may sometimes be "0B" (license number).
- Alternate ID number (REF02), usually five to ten digits long.
- A descriptive name so that your coders will recognize it in the list of alternate IDs offered on the Coding page.
You can specify as many different IDs as you like, along with a description to help you remember which is which. You can deactivate IDs that you no longer use and reactivate them at will.
If you designate one of your alternate IDs as the ☑ Default, then that ID will be automatically selected in the Coding for every claim. Otherwise -- if no alternate ID is marked as the default -- then "[None]" will be automatically selected, leaving it to the biller to choose an ID as necessary.
Sending an Alternate ID in a Claim
Once your alternate ID is configured per the instructions above, you must select it for inclusion in each relevant claim. This selection is made on the Coding page, which presents your alternate IDs in a picklist.
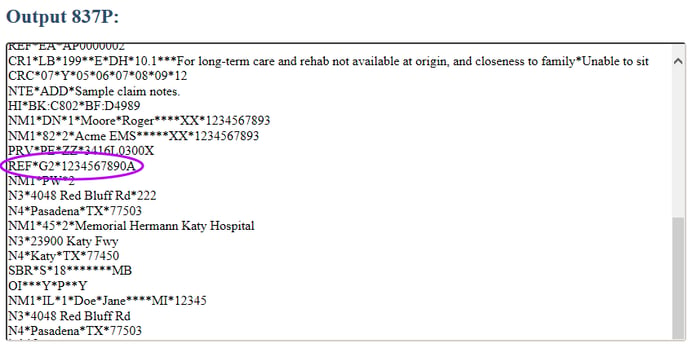
Once you select an alternate ID for a dispatch's coding, AngelTrack will include it in any X12.837P document it generates for that dispatch. You can verify it by clicking the "837P Workbench…" link on the Coding page to open the workbench to view the raw EDI data:
Configuring a Carrier for Loop 2010AA or 2010BB Workarounds
Normally an alternate ID is sent in loop 2310B REF02. A few non-compliant insurance carriers -- usually state Medicaid carriers -- require the alternate ID to be in a non-standard place: in loop 2010AA (Billing provider) or in loop 2010BB (Primary insurance payor ID). The carrier will return an error message similar to:
BILLING PROVIDER LEGACY ID Required (2010aa ref 2010bb ref)
AngelTrack can handle this situation. Visit the Insurance Payor IDs List and select the carrier's record. That will open the Insurance Payor ID Edit page, which offers the alternate ID settings plus other carrier-level workarounds:
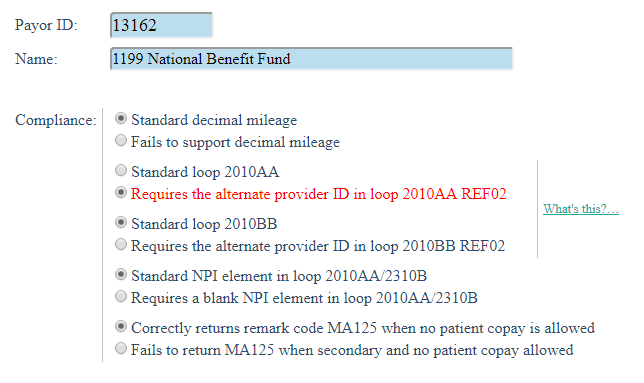
You can select one or both of the alternate ID workarounds as necessary. Once that's done, AngelTrack will engage them whenever it composes a claim intended for that insurance payor ID so long as an alternate ID was selected by the biller on the Coding page, as described in the previous section.
Using an Alternate ID as a Single NPI Billing Workaround
A couple of insurance carriers request that the NPI of the EMS company be sent in "Rendering provider" loop 2310B, even when the NPI is the same as that of the "Billing provider" sent in loop 2010AA. Beginning in the EDI 5010 specification (in 2012), loop 2310B must be omitted when the billing provider is the same as the rendering provider. This is a common situation in the EMS world: many EMS companies do their own billing under their own NPI... in which case the rendering provider loop 2310B must be omitted. And AngelTrack does so.
Unfortunately, some carriers require loop 2310B to be sent anyway, contrary to the 5010 specifications.
In order to satisfy their demand, you can force AngelTrack to send loop 2310B by specifying an alternate ID in loop 2310B REF02.