Single NPI Billing, Taxonomy Codes, and Missing Loops 2000A or 2310B
A discussion of X12/837P problems on specific clearinghouse/carriers
This article discusses an X12/837P problem seen at some clearinghouses and carriers. It has several possible causes but usually manifests as a claim rejection due to:
- Missing loop 2000A,
- Missing or wrong taxonomy code, or
- Missing loop 2310B / Missing rendering provider.
This problem is limited to those agencies who use the same NPI for billing as they do for rendering EMS services.
The problem is mostly limited to the EMS industry, with a few exceptions. The folks at Therabill have wrestled with the same issue in the broader world of medical billing. They wrote this article to describe their own workarounds for it.
Wrong Taxonomy Code
AngelTrack is usually configured with taxonomy code 3416L0300X, which is "Ambulance - Land". Depending on how your agency is enrolled, your clearinghouse and/or the carriers may want 341600000X instead, which is "Ambulance - General".
You can change your taxonomy code under the "Billing Configuration" item under the Settings page.
If you bill under a separate NPI than you render EMS services, then you must verify both taxonomy codes -- the one for rendering and the one for billing.
Missing Loop 2000A / Missing Taxonomy Code
If your clearinghouse or a carrier doesn't accept either of the aforementioned taxonomy codes, the cause may be that your enrollment (as an EMS provider) contains an error. You must also be enrolled as an organization rather than as an individual. So, call both the clearinghouse and the affected carrier and check your enrollment.
(If you are rendering services under an 'individual' NPI rather than an 'organizational' NPI, then ask your clearinghouse for advice.)
If your provider enrollment is correct, but certain carriers (notably UnitedHealthcare) are complaining about a missing taxonomy code, then the problem may be the taxonomy prefix. The prefix is specified differently in a biller/renderer situation than in a single NPI situation:
- PRV*BI for the billing provider when the rendering provider is different
- PRV*PE for the rendering provider when the billing provider is different
- PRV*PT for a single-NPI organizational provider
The PT taxonomy prefix may be inadvertently causing your clearinghouse to scrub the entire loop 2000A*PRV from your claims, which then causes the carriers to complain.
Workaround: Force "BI" prefix
If you make no progress with the clearinghouse and carrier, then there is a workaround: Force AngelTrack to always use the "BI" prefix rather than the "PT" prefix.
This can be enabled in the "Billing and rendering provider" section in the Billing Configuration page under Settings. Switch it from "Auto" to "BI", and save. Do not specify your NPI a second time under "Billing provider"; just specify it once, at the top, in the "Billing and rendering provider" section.
The setting is system-wide and will therefore affect all of your claims, but other carriers do not seem to mind the change.
Missing Loop 2310B / Missing Rendering Provider
When an organization bills under the same NPI as it renders EMS services, AngelTrack must omit loop 2310B (the rendering provider); see below for the reason why.
Consequently, if the reason for rejection is a missing loop 2310B, then you should check your enrollment at both the clearinghouse and at the affected carrier(s). Make sure your EMS operation is registered as an organization rather than as an individual, and make sure that both clearinghouse and carrier have a single, correct NPI enrolled for you.
This problem might manifest as a 277CA rejection, like this:
SSI EDIT 195112 SUITE P0PTS[5 4 2024 011543] -- WHEN BILLING FOR A GROUP THE RENDERING PHYSICIAN (2310B-NM1) IS REQUIRED. [PTSVER 04 29 2024]
Workaround: Force "BI" prefix
If your enrollments seem fine, then the problem may actually be the "PT" taxonomy prefix outlined above.
To rule that in or out as the culprit, try the "BI" prefix workaround described above.
Workaround: Switch to dual-NPI billing
If still no luck, but you want to keep your current clearinghouse anyway, then consider implementing dual-NPI billing, where your billing arm operates under its own organizational NPI, different from that used to render EMS services.
Workaround: Forcing Loop 2310B Via REF*G2
AngelTrack can be compelled to emit loop 2310B in a single-NPI situation as a workaround for a non-compliant clearinghouse or carrier.
This is accomplished using the REF*G2 mechanism, which is used to specify the rendering provider's alternate ID number. An alternate ID number can be anything, and can be assigned by anyone, for any purpose. AngelTrack permits you to input all of your alternate ID numbers and to select among them for each claim.
REF*G2 is sometimes referred to as CMS-1500 box 24j.
Because the alternate ID is specified in a REF*G2 segment within loop 2310B, if you select an alternate ID, then AngelTrack must emit the entire loop 2310B in order to include the REF*G2 segment containing the alternate ID. The clearinghouse doesn't care about REF*G2 (since it is only used by carriers), and so the claim may sail through.
To use this workaround, you must enter your company's alternate ID number(s) on the Billing Configuration page under Settings. You can specify as many different IDs as you like, along with a description to help you remember which is which. You can deactivate and reactivate your alternate IDs at any time.
Once you've created one or more alternate IDs, they will appear as a choice in the Coding page, like this:
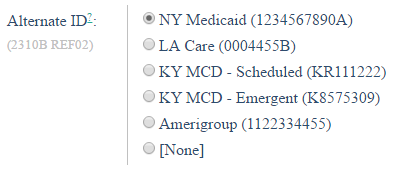
If you designate one of your alternate IDs as the ☑ Default, then that ID will be automatically selected by the Coding page for every claim, which would be appropriate if implementing this workaround at the clearinghouse level (i.e. using the workaround for all claims). Otherwise -- if no alternate ID is marked as the default -- then "[None]" will be automatically selected, leaving it to the biller to choose an ID as necessary, which would be appropriate if implementing this workaround at the carrier level (i.e. if using the workaround only for specific carriers).
Loop 2310B in the X12/5010 Standard
To better understand why AngelTrack omits loop 2310B in a single-NPI billing situation, you must look at the X12 standard, which governs the contents of 837P EDIs.
Here is the page from the actual standard explaining when loop 2310B must be present or absent:
This represents a change from the old 4010 standards. In 5010, which became law via HIPAA in 2012, the claim must not contain loop 2310B unless "the Rendering Provider information is different from that carried in Loop ID-2010AA - Billing Provider".
Because this requirement only went into force in 2012, and because it only affects single-NPI entities such as EMS providers, some clearinghouses never implemented this change in their software.
How the standard looks in practice
When an EMS provider performs its billing under a different NPI than it operates under, its claims should look like this:
EDI header
Loop 1000A: EDI sender
Loop 1000B: EDI recipient
Loop 2000A: Billing provider taxonomy (PRV*BI)
Loop 2010AA: Billing provider name, NPI, EIN
Loop 2000B: Primary insurance type
Loop 2010BA: Primary insurance subscriber
Loop 2010BB: Primary insurance name, payor ID
Loop 2300-CI: Claim settings
Loop 2300-DTP: Date of occurrence
Loop 2300-AMT: Patient copay
Loop 2300-REF: PAN, patient record number
Loop 2300-CR1: Ambulance reasons
Loop 2300-CRC: Ambulance certifications
Loop 2300-HI: Diagnosis codes
Loop 2310B: Rendering provider name, NPI, EIN
Loop 2310B-PRV: Rendering provider taxonomy (PRV*PE)
Loop 2310E: Ambulance pickup address
Loop 2310F: Ambulance dropoff address
Loop 2320: Secondary insurance type
Loop 2330A: Secondary insurance subscriber
Loop 2330B: Secondary insurance name, payor ID
Loop 2400: Procedures
EDI trailer
Whereas an EMS provider that uses the same NPI for operations and for billing must send claims like this:
EDI header
Loop 1000A: EDI sender
Loop 1000B: EDI recipient
Loop 2000A: Rendering provider taxonomy (PRV*PT)
Loop 2010AA: Rendering provider name, NPI, EIN
Loop 2000B: Primary insurance type
Loop 2010BA: Primary insurance subscriber
Loop 2010BB: Primary insurance name, payor ID
Loop 2300-CI: Claim settings
Loop 2300-DTP: Date of occurrence
Loop 2300-AMT: Patient copay
Loop 2300-REF: PAN, patient record number
Loop 2300-CR1: Ambulance reasons
Loop 2300-CRC: Ambulance certifications
Loop 2300-HI: Diagnosis codes
(Loop 2310B omitted)
Loop 2310E: Ambulance pickup address
Loop 2310F: Ambulance dropoff address
Loop 2320: Secondary insurance type
Loop 2330A: Secondary insurance subscriber
Loop 2330B: Secondary insurance name, payor ID
Loop 2400: Procedures
EDI trailer
AngelTrack implements this standard exactly.
The problem is that sometimes the clearinghouse and/or the carrier doesn't understand that an EMS organization is the biller and the renderer.
Clearinghouses and carriers are accustomed to how doctor's offices file their claims. In a doctor's office, the overall practice is the billing provider (i.e. the office that does the billing), and then the individual doctors are the rendering providers (i.e. the people who actually treat patients). So when EMS sends a claim in which the EMS organization is the biller and the renderer, they think it's a mistake.
The 5010 specification adopted in 2012 makes allowance for EMS providers in this situation, but that provision has not been fully implemented by all billing software.
Why is this problem limited to EMS providers?
The issue of single NPI billing is mostly limited to EMS providers because other healthcare organizations utilize "Group NPI" billing like this:
- Billing provider: Acme Clinic using a type 2 (organizational) NPI 1111111111
- Rendering provider: Dr. John Doe using a type 1 (individual) NPI 2222222222
- Rendering provider: Dr. John Smith using a type 1 (individual) NPI 3333333333
- Rendering provider: Dr. Michael Scott using a type 1 (individual) NPI 4444444444
- Rendering provider: Dr. Mark Smith using a type 1 (individual) NPI 5555555555
Even a single-doctor practice may be structured this way:
- Billing provider: Michael Scott Medical Practice LLP using a type 2 (organizational) NPI 1111111111
- Rendering provider: Dr. Michael Scott using a type 1 (individual) NPI 2222222222
Alternatively, a single-doctor practice can actually bill its claims under a single NPI:
- Billing provider: Dr. Michael Scott using a type 1 (individual) NPI 2222222222
- (Rendering provider omitted because same as Billing provider)
...but that is very different than how a single NPI EMS provider will bill its claims:
- Billing provider: Acme EMS using a type 2 (organizational) NPI 1111111111
- (Rendering provider omitted because same as Billing provider)
As a result, most clearinghouses never encounter an EMS-style claim, a claim whose billing provider and rendering provider are a single organization rather than a single individual.
Which taxonomy code should I choose for my registration?
Here are your choices:
- 341600000X - Ambulance, General
- 3416L0300X - Ambulance, Land
We have many agencies using either code; as far as we can tell, it makes no difference to the carriers. Just make sure that whichever code you register is correctly noted on your enrollments, and in your AngelTrack server's billing configuration.
