PCS Form Requirements for EMS Transport in AngelTrack
How AngelTrack's automatic ePCS form implements some of these requirements to improve your workflow
Federal regulation 42 CFR 410.40 (COVERAGE OF AMBULANCE SERVICES) specifies how ambulance services are billed to Medicare/Medicaid, including the requirements for a "Physician Certification Statement" -- better known as a PCS document.
This is Not Legal Advice
This document is not legal advice, and AngelTrack LLC does not provide legal counsel. This document is not a full or sufficient treatment of the subject. This document is not a substitute for professional legal advice.
These regulations are expressed in AngelTrack's ePCS form and in the Prior Authorization Queue's report of missing PCS forms.
PCS Form Basics
The "Physician Certification Statement" form is used to prove medical necessity for stretcher transport.
PCS forms are required for non-emergent stretcher transports that will be covered by Medicare or by other federally-funded programs... including Medicare HMOs administered by commercial carriers.
PCS forms are not required by commercial insurance carriers (other than Medicare HMO plans). That said, a PCS form would be an effective counterargument if a commercial carrier were to deny an insurance claim based on medical necessity.
And just to repeat: they are never required for emergent transport.
AngelTrack will automatically prompt your crews to collect a PCS signature while on-scene, whenever the patient's insurance is unknown or is known to be Medicare.
There are many rules concerning who can sign the PCS form, and how long the form remains valid. Keep reading.

Federal Regulations
First, the official regulations. CFR section 410.40 lays out the cases where PCS documents are required (as of 2014 publication):
-
Medical necessity requirements
- [...]
-
Special rule for nonemergency, scheduled, repetitive ambulance services.
- Medicare covers medically necessary nonemergency, scheduled, repetitive ambulance services if the ambulance provider or supplier, before furnishing the service to the beneficiary, obtains a written order from the beneficiary’s attending physician certifying that the medical necessity requirements of paragraph (d)(1) of this section are met. The physician’s order must be dated no earlier than 60 days before the date the service is furnished.
- In all cases, the provider or supplier must keep appropriate documentation on file and, upon request, present it to the contractor. The presence of the signed physician certification statement does not alone demonstrate that the ambulance transport was medically necessary. All other program criteria must be met in order for payment to be made.
-
Special rule for nonemergency ambulance services that are either unscheduled or that are scheduled on a nonrepetitive basis.
Medicare covers medically necessary nonemergency ambulance services that are either unscheduled or that are scheduled on a nonrepetitive basis under one of the following circumstances:
- For a resident of a facility who is under the care of a physician if the ambulance provider or supplier obtains a written order from the beneficiary's attending physician, within 48 hours after the transport, certifying that the medical necessity requirements of paragraph (d)(1) of this section are met.
- For a beneficiary residing at home or in a facility who is not under the direct care of a physician. A physician certification is not required.
- If the ambulance provider or supplier is unable to obtain a signed physician certification statement from the beneficiary's attending physician, a signed certification statement must be obtained from either the physician assistant (PA), nurse practitioner (NP), clinical nurse specialist (CNS), registered nurse (RN), or discharge planner, who has personal knowledge of the beneficiary's condition at the time the ambulance transport is ordered or the service is furnished. This individual must be employed by the beneficiary's attending physician or by the hospital or facility where the beneficiary is being treated and from which the beneficiary is transported. Medicare regulations for PAs, NPs, and CNSs apply and all applicable State licensure laws apply; or,
- If the ambulance provider or supplier is unable to obtain the required certification within 21 calendar days following the date of the service, the ambulance supplier must document its attempts to obtain the requested certification and may then submit the claim. Acceptable documentation includes a signed return receipt from the U.S. Postal Service or other similar service that evidences that the ambulance supplier attempted to obtain the required signature from the beneficiary's attending physician or other individual named in paragraph (d)(3)(iii) of this section.
- In all cases, the provider or supplier must keep appropriate documentation on file and, upon request, present it to the contractor. The presence of the signed certification statement or signed return receipt does not alone demonstrate that the ambulance transport was medically necessary. All other program criteria must be met in order for payment to be made.
Definition of "repetitive"
You may have noticed the critical term "repetitive" in the regulations. So what exactly is a repetitive transport under the law?
CMS Program Memorandum AB-03-106 defines "repetitive":
A repetitive ambulance service is defined as medically necessary ambulance transportation that is furnished three or more times during a 10-day period or at least once per week for at least three weeks. Dialysis and respiratory therapy are types of treatments for which repetitive ambulance services are often necessary. However, the requirement for submitting the PCS form for repetitive, scheduled, non-emergency ambulance services is based on the quantitative standard (three or more times during a ten-day period or at least once per week for at least three weeks). Similarly, regularly scheduled ambulance services for follow-up visits, whether routine or unexpected, are not "repetitive" for purposes of this requirement unless one of the quantitative standards is met. PCS requirements for other types of ambulance transports are specified in PM AB-03-007.
Definition of "emergency"
Because emergency transports do not require PCS forms, it is important to know exactly what qualifies as emergent transport.
The Medicare Benefit Policy Manual Chapter 10 states:
Emergency response is a BLS or ALS1 level of service that has been
provided in immediate response to a 911 call or the equivalent. An immediate response is one in which the ambulance provider/supplier begins as quickly as possible to take the steps necessary to respond to the call.
The term "emergency" refers only to the fact that EMS begins to respond immediately. It does not require lights, sirens, or speeding. It does not even require that an ambulance rolls immediately, if all units are busy. "Emergent" requires only that EMS agrees and intends to respond as quickly as possible.
Although the definition of "emergency" does not specify criteria for the patient's condition, or for the type of destination, such criteria are implied by the fact that the patient needs an immediate EMS response. Therefore, if the patient is not in condition yellow or red, or if the destination is not a hospital ER, then be very cautious about dispatching or billing the trip as emergent.
In AngelTrack, the dispatcher indicates the emergence of the response via the priority control:
![]()
The control is designed to correspond to the CMS meaning of "emergent". Thus, the "Lower acuity" priority level means EMS is not responding as soon as possible; instead, the patient can wait until all emergent patients have been serviced first.
Executive summary of the regulations
The regulations as written allow for the following types of PCS in the four circumstances of EMS stretcher transport:
| Trip type | Physician signature | Proof of attempt to contact physician | PA, NP, CNS, RN, or discharge planner | |
|---|---|---|---|---|
| Non-emergency transport | Unscheduled | ✔ | ✔ | ✔ |
| Scheduled, non-repetitive | ✔ | ✔ | ✔ | |
| Scheduled, repetitive | ✔ | ✘ | ✘ | |
| Emergency transport | [No PCS is required] | |||
AngelTrack's built-in ePCS form knows these regulations and will exactly apply them when operating in ☑ Strict mode. We will learn more about AngelTrack's PCS modes further below.
Using AngelTrack to Document an Attempt to Collect a PCS
In AngelTrack it is easy to document an unsuccessful attempt to collect a signed PCS form. You will need a scan or photograph of the envelope showing its Certified Mail coupon, plus a scan or photograph of the blank PCS form that was mailed. Attach those two scans to a new electronic document in AngelTrack, using the Patient Document Upload facility under Billing Home.
When creating the document, take care to specify the exact destination approved by the physician (e.g. the exact dialysis facility). For the start date, specify the date you mailed the form to the doctor. For the end date, specify exactly 60 days into the future from the start date.
Once that's done, then your two scans (the envelope and the form) will automatically appear inside the run report for each trip the patient makes to or from the selected destination, within the date range you specified.
Choosing a PCS Completion Mode in AngelTrack
The Preferences page under Settings offers three PCS Completion modes to match your company policy:
- ☑ Advisory notifies the crew that a PCS is needed, but allows them to send their report onward to QA without providing one. If the ePCS is signed by a PA, NP, CNS, RN, or discharge planner, the document will be valid only for the round trip; if signed by a physician, the document will be valid for a date range specified in the form -- up to the 60-day limit imposed by the CFR.
- ☑ Strict implements 42 CFR §410.40(d)(2)(i) exactly, meaning the ePCS form will not accept a signature from a PA, NP, CNS, RN, or discharge planner when the trip is recurring. Beyond this, the "Strict" setting is the same as "Advisory"; the crew will not be required to provide a signed PCS because the crew will often be unable to find the patient's physician.
- ☑ Required implements "Painting a Picture" by requiring a PCS or ePCS from the crew for all non-emergency stretcher trips for all Medicare patients. The crew is not permitted to send their report onward to QA until one is provided (or is attached by a biller). If the ePCS is signed by a PA, NP, CNS, RN, or discharge planner, the document will be valid only for the round trip; if signed by a physician, the document will be valid for a date range specified in the form -- up to the 60-day limit imposed by the CFR.
- ☑ Always is the same as "Required" with one exception: a PCS or ePCS will be required from the crew for any insurable BLS+ transport, instead of just for Medicare patients. Use this option if your crews are disobediently setting every patient's insurance type to "[None]" in order to bypass the PCS collection requirement.
- ☑ Never is only for use by EMS firms outside of the United States of America.
Do not change your PCS completion mode without first consulting your legal team and/or someone with experience in demonstrating compliance to a Medicare auditor.
AngelTrack's PCR will guide the crews
Your PCS completion mode setting will be put into practice by AngelTrack's PCR, which uses dark yellow and bright yellow indicators to show the attending that a PCS is requested or demanded, respectively.
To learn more about how the PCR uses color to guide the attending through report completion, read the Report Writing guide.
PCS Coverage Reports
AngelTrack's reports show what fraction of your transports have the necessary PCS, and which do not.
Under Billing Home there are two reports: the general PCS Coverage which shows across-the-board percentages, and the PCS Coverage By Facility which breaks out the percentages by origin facility.
Both reports break out the numbers like this:
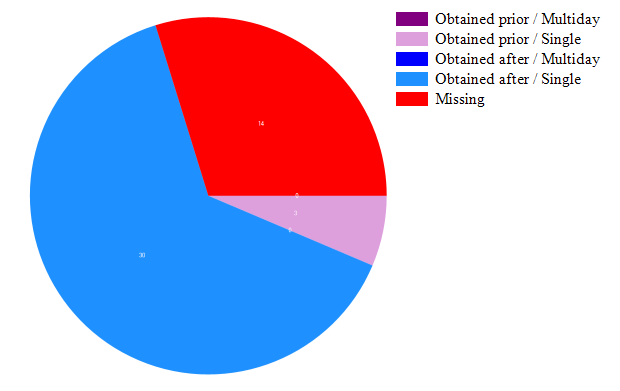
"Obtained prior" means the PCS form -- be it electronic, or be it a scanned paper form -- was recorded in AngelTrack prior to the date/time of service. A high number of "obtained prior" PCS forms is a good indicator for your billing office.
"Obtained after" means the PCS form was recorded in AngelTrack on the day of service or at some point afterward.
The PCS Coverage By Facility report shows you which facilities have the most PCS coverage gaps, so that you can arrange a visit to get caught up:
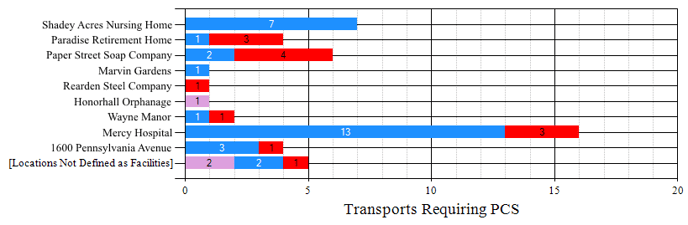
The row labelled "[Locations Not Defined as Facilities]" refers to origin addresses that were not stored as facility records in AngelTrack. You can still attach PCS documents to these dispatches, but they cannot be covered by multi-day PCS documents because multi-day PCS documents are indexed by destination facility.
Retroactive PCS Signatures
Federal regulations do not give any guidance for PCS signatures collected after the date of service. Therefore it is up to your region's MAC to publish guidelines about who can sign a retroactive PCS, and how far back in time the form can go.
If in doubt, consult your legal team. If you do not have a legal team, or if your legal team is not experienced in matters of Medicare compliance, then consult Page, Wolfberg, and Wirth EMS Law Firm.
Also keep in mind: just because your MAC does not specifically recognize a retroactive PCS signature, doesn't mean the signature has no value. It can still be part of "painting the picture" of medical necessity, and it can still help signal your organization's positive attitude towards compliance.
Visiting a Facility to Collect Many PCS Signatures At Once
The aforementioned reports will show you which facilities are missing the PCS paperwork for upcoming transports, as well as for recently completed transports.
You can visit the facility and take a tablet computer with you, to knock out many PCS forms in one sitting. To learn how, read the Bulk PCS Form Collection Guide.