Filing a Coded Claim
How to file a completely coded claim in AngelTrack / How to send a coded claim your clearinghouse.
AngelTrack's post-process workflow supports both in-house and outside billers. This help document is for in-house billers and for outside billers who choose to integrate (i.e., who choose to use AngelTrack remotely to perform billing on the customer's behalf).
If you are not yet familiar with the numbers 837P, 999, 277CA, and 835, or if you do not yet know how your billing software, your clearinghouse, and the insurance carriers all work together, then read the EDI Primer first.
Calls Must be Coded First
As we know, dispatches must first be coded before submission to the clearinghouse.
Coding in AngelTrack is fast and easy since many of the data fields are filled in for you, but every field must be meticulously reviewed, as AngelTrack is not a CAC, and, thus, cannot code a claim for you.
Here are the prerequisite steps to prepare an insurance claim to be billed:
- The trip must be marked as ☑ Bill insurance, else it will go straight to invoicing, bypassing entirely the insurance claim process. To learn more, refer to the Bill-To Settings Guide.
- The trip must be closed, and not as a cancellation. To learn more, refer to the Call Completion Guide. By the way, you can code and claim trips that were delegated to an affiliate but billed at your agency, if that is how the affiliate's billing settings are configured.
- The crew must finish their report in the PCR. To learn more, refer to the EMS Report Writing Guide.
- The crew must satisfy all State Data Validation Rules that apply to the service provided, and then submit their report to QA.
- The QA reviewer must pass (graduate) the report. To learn more, refer to the QA Review Guide.
- When the trip appears in the Insurance Review Queue, the insurance reviewer must decide to claim the trip with insurance, rather than sending it straight to invoicing. To learn more, refer to the Insurance Review Queue Guide.
- When the trip appears in the Insurance Filing Queue, the coder must click the "Not yet coded" link to open the Coding page and perform the coding. To learn more, refer to the Coding Guide.
Gathering Claims into a Batch
From the Insurance Filing Queue, tick the ☑ checkboxes in the leftmost column of the grid, selecting items for inclusion in a claim batch. Your clearinghouse can handle batches containing a mixture of Medicare, Medicaid, and Private claims... but your batches will probably be easier to manage if they contain only a single type of carrier.
Once you've chosen the items for the batch, click "Batch the Checked Runs" from the "Bulk Operations" box. As you create each batch, AngelTrack automatically generates the necessary "Claim Filed" payment events.
The underlying dispatches will then exit the Insurance Filing Queue, moving to "Awaiting payment". Meanwhile, your web browser will be redirected to the Insurance Transmission Queue where you can see your new batch.
To learn more about 837P batches in AngelTrack, refer to the Managing 837P Claim Batches Guide.
Sending a single claim
Instead of gathering claims into a batch, you have the option to transmit a single claim, right from the Coding page.
Once the coding is ready, scroll down and instead of clicking "Save", click "Save and Batch". AngelTrack will save your work, place it into a single-claim batch, and place the batch in the outgoing queue.
Transmitting the Batch to the Clearinghouse
The Insurance Filing Queue produces batches of claims which are ready to go to your clearinghouse. Other billing queues can also create batches.
After you create a batch, AngelTrack will redirect you to the Insurance Transmission Queue where you can see your new batch. To view its contents or cancel it, click the batch's ID to open the EDI Batch Edit page.
If AngelTrack's clearinghouse uploader/downloader is active, then it will automatically transmit your batch to your clearinghouse -- normally within 60 seconds. When that happens, the batch will change from Pending upload to Transmitted, and all included dispatches will then exit the Insurance Filing Queue / Insurance Exception Queue, allowing you to move on to the next trips that you intend to claim. The uploaded batch, meanwhile, awaits the return of an X12.999 acknowledgment from your clearinghouse, which, when it arrives, will automatically mark the batch as Accepted or Rejected.
Whereas if you do not use the clearinghouse uploader/downloader, then refer to the Clearinghouse Manual EDI Upload/Download Guide to learn how to do this manually.
CMS-1500 / Paper claims
From the Insurance Transmission Queue, you can download a claim batch as a PDF containing a set of CMS-1500 documents, one per claim. You can then mark the batch as "transmitted" in the usual way.
You can also download single CMS-1500 forms from the Insurance Filing Queue, as well as from other billing queues. If you do so, and if you submit the 1500 to a carrier, then be sure to click the "Record Claim Filed Events" button, which tells AngelTrack that you've filed the claim.
If AngelTrack's clearinghouse uploader/downloader is active, then you must prevent it from uploading the claim batch that you intend to print as 1500s. To do this, select the "Claim batch (not for upload)" option when batching.
To learn more, refer to the Filing a Paper Claim Guide.
Unsupported clearinghouse
If your clearinghouse rejects one of AngelTrack's 837P documents, then contact AngelTrack Support. Every clearinghouse has requirements for its 837Ps, and so every clearinghouse produces an "837P Companion Guide" detailing these requirements. If you provide that guide to AngelTrack Support, they will review it and give you a timeline for implementing it. That way you won't need to switch clearinghouses.
Processing the Clearinghouse's Reply
Your clearinghouse should reply with an X12.999 document, which is an electronic data file that tells AngelTrack whether the batch of claims was accepted or rejected. If the batch was rejected, the data file will include an explanation.
If active, AngelTrack's clearinghouse uploader/downloader will fetch these replies from your clearinghouse and attempt to import them automatically. Whereas if you do not use the clearinghouse uploader/downloader, then refer to the Clearinghouse Manual EDI Upload/Download Guide to learn how to do this manually.
Upon import, a 999 will change the status of a claim batch from "Transmitted" to either "Accepted" or "Rejected".
999 rejections
If the 999 document is a rejection, then all of the claims in the batch will be marked "failed", and all of the dispatches in the batch will go back to the Insurance Filing Queue (or Insurance Exception Queue if that's where they were before) to be re-coded and re-batched.
In that event, the Coding page will have a "Last 999" tab that you can click to see why the batch was rejected.
To learn more, refer to the 837P Batch Management Guide - 999 Section.
Processing the Replies from the Carriers
The insurance carriers should reply with X12.277CA documents, which are electronic data files that tell AngelTrack which individual claims are accepted for adjudication versus which are rejected. Your clearinghouse will collect the 277CA documents from the carriers and make them available to you for download.
If active, AngelTrack's clearinghouse uploader/downloader will fetch these replies from your clearinghouse and attempt to automatically import them. Whereas if you do not use the clearinghouse uploader/downloader, then refer to the Clearinghouse Manual EDI Upload/Download Guide to learn how to do this manually.
AngelTrack will process each 277CA document looking for rejections. Any rejected claim will be marked as such*, and then its dispatch will go back to the Insurance Filing Queue (or Insurance Exception Queue if that's where it was before) to be corrected and re-batched. When that happens, the Coding page will have a "Last 277CA" tab which you can click to see the reason for rejection.
Rejections from carriers are common and occur for all sorts of reasons including an invalid patient ID number, invalid group number, invalid SSN or DOB, expired policy, invalid diagnosis codes, missing modifiers, etc., etc.
To learn more, refer to the 837P Batch Management Guide - 277CA Section.
*When a claim is rejected by the clearinghouse or by a carrier, the corresponding "Claim" payment event in AngelTrack will be marked "failed", and the relevant 999 or 277CA document will be attached to the payment event for review.
EOBs Will Arrive Later
About a week or two later, X12.835 EOBs will come back from the carriers through your clearinghouse.
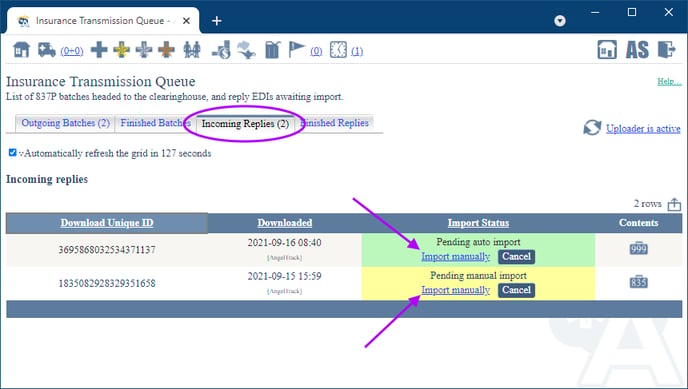
If active, AngelTrack's clearinghouse uploader/downloader will fetch these for you, depositing them into the "Incoming Replies" tab of the Insurance Transmission Queue. Whereas if you do not use the clearinghouse uploader/downloader, then refer to the Clearinghouse Manual EDI Upload/Download Guide to learn how to do this manually.
After download, AngelTrack will automatically import some of them... but any EOB that contains denials or corrections, or ambiguous information, will be left to a biller to manually review and import. These EOBs will be marked "Pending manual import" and remain in the "Incoming Replies" tab until a biller imports them.
To learn more, read the Importing EOBs guide.
Manual input of paper EOBs
If your clearinghouse does not provide EOBs in X12.835 format, then you must manually record them in AngelTrack. Each claim line in the EOB should become a payment event that reflects the insurer's reply. These payment events then drive AngelTrack's post-process workflow. To learn more, refer to the Reading a Paper EOB Guide.