Coding / Code an Insurance Claim
A complete walkthrough of everything relating to coding a claim on AngelTrack
Coding is the last step before filing an insurance claim in AngelTrack. The Coding page, accessible from the Insurance Filing Queue, is built to make coding quick and easy.
You can take advantage of the coding features even if not using AngelTrack to file your insurance claims: once coded, dispatches can be exported in X12.837P format for upload or import elsewhere.
If you are not yet familiar with the numbers 837P, 999, 277CA, and 835, or if you do not yet know how AngelTrack talks to your clearinghouse and the insurance carriers, we recommend reading the EDI Primer first.
"Is this all there is?"
If you are migrating to AngelTrack from other billing software, you may find yourself wondering "Is this all there is?" After all, most billing software contains dozens and dozens of data fields that must be filled in, from scratch, for every call.
The answer is yes, this really is all there is to code an EMS transport for filing. AngelTrack already has most of the information needed to bill the call stored in the dispatch and PCR records. Because the data is vertically integrated, billers need not retype anything. Most of the 837P no longer requires manual intervention.
AngelTrack is not general-purpose medical coding software. It is not able to code for a doctor's office call, a CT scan, or a dose of chemotherapy. It is only for EMS transports.
837P Loop Numbers / CMS-1500 Box Numbers
To see how CMS-1500 box numbers match up to X12.837P loop numbers, and to see from where AngelTrack draws each box's data, read the AngelTrack CMS-1500 Crosswalk document.
That crosswalk lists every box on the 1500 and explains how AngelTrack populates it with data.
Patient Demographics
The demographic data on file for the patient is pre-loaded into the data fields, ready for final edits before claim filing. If some data is missing, you can switch to the "Librarian" tab to pull up a recent face sheet for the patient.
If your demographic data is regularly missing, we recommend using the Missing Demographics Queue.
Remember that the "Patient weight" field is checkpointed, meaning that edits to the field do not necessarily propagate to the patient's other calls.
Service Facility Location / Loop 2310C
The service facility location goes in box 32a of a CMS-1500, or in loop 2310C of an X12.837P electronic claim.
This information is required only by certain insurance carriers; most carriers don't request it, because an ambulance claim already includes the pickup address in loop 2310E and the dropoff address in loop 2310F, and therefore the "service facility" is assumed to be the ambulance itself.
So, for most claims, you will leave this coding option set to "Normal / Implicit".
For those carriers who do want to receive box 32a / loop 2310C, they want the name, address, and NPI of the hospital to which the patient was transferred. AngelTrack will offer you the choice to send the origin facility or the destination facility... but only if all of the following are true:
- The dispatch record has got facility records attached as its origin/destination; and
- The attached facility record(s) specify their NPI.
Mileage
If actual odometer readings are available from the crew, then the ☑ Actual mileage will be displayed and pre-selected for the claim. AngelTrack will also display the normal mileage for the route if known, for comparison to assist you in identifying an error in the actual odometer readings.
Normal mileage is a system in AngelTrack to help identify missing or wrong actual mileages. Make sure you understand it before using it for coding; read the Mileage guide to learn more. If the actual mileage is missing or wrong, we strongly recommend sending the call back for correction instead of filing with normal mileage.
If you do file ☑ Normal mileage, the mileage value will be "frozen" when you file the primary claim. Any secondary claim will use the same mileage value, even though the statistically-derived normal mileage may have drifted since then.
Declared mileage
If there is a declared mileage on file for the route, the declared value will appear as the ☑ Normal mileage selection. Saving that as your choice will then freeze the declared value for the claim, as discussed. If you later modify the declared mileage, and want to use the new declared value for your claim, you must unfreeze the current data by switching the claim to ☑ Actual mileage and saving, then return to the Coding page and re-select ☑ Normal mileage.
Medically unnecessary mileage
If the patient demanded transport farther than to the closest appropriate medical facility, you might choose to code the necessary mileage (to the closest appropriate facility) separately from the unnecessary additional mileage. There is an option to declare this mileage as ☑A0888 under the "Additional service codes" section of the page. AngelTrack will then automatically subtract the unnecessary mileage from the total transport distance to compute the claimed amount of necessary mileage.
Prior Authorization / Loop 2300*REF*G1
The prior authorization number is included in the electronic (X12.837P) insurance claim. There may be one or more PAN documents on file that apply to the current call; AngelTrack will search for applicable PAN documents like this:
- Find any documents of type 'PAN' or 'McPAN' that are attached directly to the trip, where the "Comments" field was filled in (presumably with an authorization number).
- Likewise find any 'PAN' or 'McPAN' documents attached directly to the paired dispatch, if any. The term "paired dispatch" means the return trip attached to an outbound trip and vice versa.
- Find any documents of type 'PAN' or 'McPAN' that are attached to the patient and which match this trip's date of service and its origin or destination facility, and which have a "Comments" field filled in.
All such matching documents are listed in the drop-down list of PANs on the Coding page, allowing you to choose the one with a usable authorization number. You also have the option to hand-type the authorization number.
You may need to review the actual PAN document page scans in order to discover the authorization number; this is where the "Librarian" tab comes in handy. The Coding page's "Librarian" tab shows all documents that apply to the current call, including PAN documents. You can use it to quickly view all applicable documents to find the correct PAN.
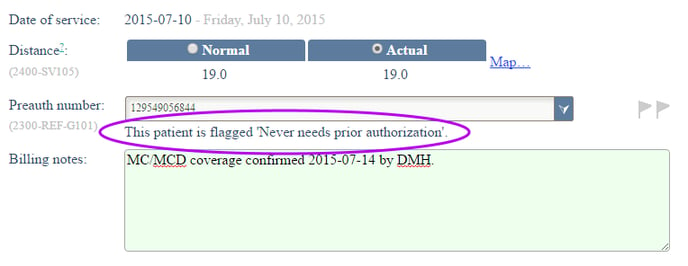
Patients with special PAN requirements
Remember that a patient record can be flagged as ☑ Always requires prior authorization or ☑ Never requires prior authorization.
If either flag is set, the Coding page will indicate it with a message adjacent to the "Preauth number" field, like this:
Claim Settings
The "Claim Settings" radio buttons allow you to control certain fields in the 837P:
Original, Refile, or Replacement
☑ Original creates an ordinary claim: BHT02 [Transaction Set Purpose Code] will be set to "01" and CLM05-3 [Claim Frequency Code] set to "1".
The claim control number will be generated using the underlying dispatch ID plus the number of times the call has already been filed. For example, the claim control number for the first time that dispatch ID 1234 is filed will be AD + 1234 + N1. The N1 means "number 1 claim", so you may sometimes see N2, N3, N4, and so forth. To learn more about AngelTrack's EDI control numbers, read AngelTrack's EDI Control Numbers guide.
☑ Refile is the same as "Original", but each time the 837P is generated, regardless of whether for primary or for secondary, it will carry the same claim control number as before. This is done to avoid confusion with secondary documentation in the event that a claim is refiled; if the claim control number changed each time it was refiled, then additional documentation bearing the original claim control number would not match that of the refiled claim.
This setting will be automatically selected once a claim is filed so that any re-filings or secondary filings will all carry the same control number. If your clearinghouse or if an insurer requires a claim to be refiled using a different claim control number, then select ☑ Original instead.
☑ Replacement creates a claim with BHT02 [Transaction Set Purpose Code] equal to "18" rather than "01" and CLM05-3 [Claim Frequency Code aka box 22] equal to "7" rather than "1", for the purpose of filing a correction claim against a claim already filed previously. The claim control number from the original filing will be reused.
When emitting a replacement claim, AngelTrack will include -- in loop 2300 REF/F8, and in CMS-1500 box 22 -- the most recent payor control number received from the carrier. This is also known as an "original reference number." You can check whether AngelTrack has one on file -- it will appear on the Coding page in the claim status table shown just below the Primary / Secondary selector.
Check with your clearinghouse before attempting to file a replacement claim, as some carriers -- including all the MACs -- accept only original chargeable claims. If you are not sure whether a carrier accepts replacement claims, call their support line or perform an internet search for their "837 Companion Guide".
AngelTrack cannot emit cancellation claims (CLOM05-3 set to '8'); if you need to cancel a claim, you must do so using your clearinghouse's user interface.
Chargeable or Report
☑ Chargeable creates a normal claim, setting BHT06 to "CH".
☑ Report only creates an "encounter" claim, setting BHT06 equal to "RP", for the purpose of reporting a service performed without also demanding payment. Check with your clearinghouse before using this setting.
Assignment of benefits
☑ Pay directly to EMS will set CLM08 to "Y", directing the insurer to pay benefits directly to EMS. The patient will receive an EOB and, if applicable, a notice of copay due.
☑ Pay to the patient will set CLM08 to "N", directing the insurer to pay benefits to the patient, rather than to EMS. EMS must then bill the patient for any balance owing.
Price schema
If you wish to claim a price other than retail, you may select one of the purple (patient) rates instead. The purple rates are configurable using the Pricing page under Billing Home.
We strongly recommend against submitting any rates other than retail to any insurer without first consulting your legal counsel to understand the compliance issues involved. Many insurers now have one or more government-funded plans, and charging such a plan a higher rate than that charged to other insurers may create a legal hazard... even if both insurers may ultimately adjudicate the same amount.
File against
☑ Secondary insurance will generate an 837P for the secondary insurer that automatically includes all the information returned in the 835 from the primary insurer. This includes all amounts claimed, all amounts paid, and all adjustment reasons and amounts. This information is communicated in the 2430 loop that accompanies each 2400 loop (i.e. that accompanies each service line).
In order for the aforementioned to work correctly, you must import the electronic EOB (i.e. the X12.835) from the primary insurer first... or if the primary's EOB was paper, then the EOB's adjustments chart must be input into AngelTrack. When input, the claim and benefit information will appear as a brief summary underneath the ☑ Primary insurance radio button.
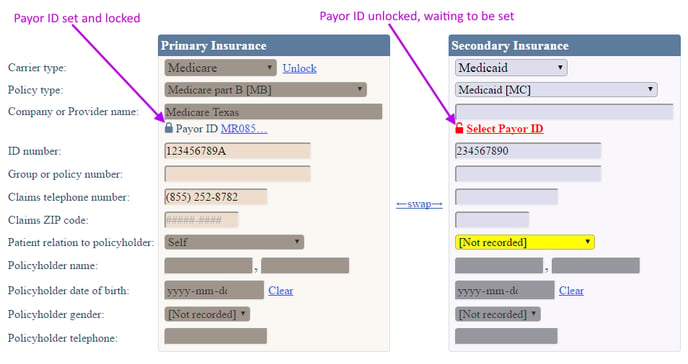
Patient Insurance and Payor IDs
The Coding page gives a final opportunity to revise the patient insurance fields prior to filing the claim. Remember that any changes to the insurance fields are applied only to the relevant patient data checkpoint... but you can tick the ☑ All checkpoints on or after checkbox to apply your changes over a date range.
You can easily switch to the "Librarian" tab to pull up the patient's face sheet, or a scan of their insurance cards, if such documents are on file and if they apply to the current call.
In any event, you must select insurance payor IDs if that has not already been done. Click the red "Select Payor ID" link to open the payor ID selection popup window, as necessary. You can then search, sort, and filter the list until you find the one you need.
Once set, the payor ID will be carried forward through all of the patient's future calls... until somebody clicks the "Change" button to force the payor ID to be selected again.
Reviewing and updating the payor ID list
AngelTrack has a built-in list of payor IDs from your clearinghouse. When AngelTrack was first deployed, the administrator configuring your server downloaded the latest list from your clearinghouse and then imported it.
Your clearinghouse updates its payor ID list from time to time and posts the latest version on its website. About once a year, we recommend downloading the latest list and importing it into AngelTrack, so that you'll have access to the latest data.
To learn more about the insurance payor ID list, read the Insurance Payor ID List Guide.
Crews can clear the payor ID
When a crew runs a call and opens the PCR, they have the opportunity to review the patient's insurance information. If a payor ID has been set for the patient, then the controls for "Insurance Type" and "Insurance Provider Name" will be locked. If the crew -- looking at a face sheet -- decides that the locked fields are incorrect, they can click the "Change" button and make changes. When they do so, the old payor ID is discarded. The crews input the insurance type and the provider's name, but only a biller can re-select the payor ID.
Therefore you must train your crews to use the "Change" button only if they are certain that their face sheet is up-to-date and only after double-checking that the current payor ID is wrong.
AngelTrack has a built-in announcement explaining this to your crews. After reviewing and editing the announcement to fit your organization, you can activate it to disseminate this bit of training.
Setting the policy type / SBR09
The policy type field governs the contents of loop 2000B segment SBR09. It is usually not necessary to specify the policy type because AngelTrack infers the policy type from the carrier type:
| Carrier type | Policy type inferred | 837P element SBR09 | CMS-1500 box 1 |
|---|---|---|---|
| None | Self-pay | 09 | (no boxes checked) |
| Private | Commercial Insurance | CI | ☑ GROUP HEALTH PLAN |
| Medicare | Medicare part B | MB | ☑ MEDICARE |
| Medicaid | Medicaid | MC | ☑ MEDICAID |
| Other government | Another federal program | OF | ☑ OTHER |
| Workers Comp | Workers' Compensation | WC | ☑ OTHER |
Of course, you can override the inference by setting the appropriate policy type according to the carrier's instructions or their 837P Companion Guide. You must set the policy type before locking the payor ID, as you will not be able to edit the policy type once it is locked.
Group number / Benefit indicator / SBR03
If a carrier asks for a "Benefit indicator" in loop 2000B element SBR03, place the necessary data in the "Group or policy number" box of the patient's insurance.
Other Insurance Policy Type / SBR05
Element SBR05 in loop 2000 and in loop 2320 is normally left blank. However, if Medicare is the secondary carrier, then SBR05 must contain the reason why Medicare is not the primary.
To satisfy this requirement, the biller must use the Policy Type field on the secondary insurance to indicate the reason why Medicare is not the primary. AngelTrack then emits this answer in SBR05.
If you get a rejection or denial due to missing SBR05, then check that the Insurance Policy Type field is set correctly for each carrier.
Diagnosis Codes
AngelTrack can assist you in selecting the most accurate diagnosis codes for each transport.
Autocomplete (typeahead) helpers
All six of the diagnosis-code textboxes on the Coding page have to autocomplete (aka typeahead) helpers for you, which search the entire ICD-10 code library for codes that match what you've typed.
These helpers are aware of which ICD-10 codes have a "7th character extension" and will offer all permitted extensions to any code you type. For example, if you type "S21.03", AngelTrack will offer you the three permitted derivatives: S21.03XA, S21.03XD, and S21.03XS. Using the autocomplete helpers will thus ensure that you never forget to include a required 7th character.
AngelTrack's index of recommended codes
AngelTrack has about 1,000 ICD-10 codes available in a recommended-codes index. The contents of the index are:
- The 296 codes suggested for EMS transports by Novitas;
- About 600 codes suggested for ambulance use by a major insurance carrier; and
- About 75 codes drawn from AngelTrack historical data for claims successfully paid by Medicare.
These recommendations appear in the results displayed by the search box that sits just to the right of the Coding page's diagnosis-code fields. As you input part of a diagnosis code, or part of its description, the autocomplete helper will show you the codes that match it. For each matching code, AngelTrack will display an additional symbol:
- A two-way double arrow ⇔ if the code is recommended by Novitas for outbound and return trips
- A right double arrow ⇒ if the code is recommended by Novitas for outbound trips
- A left double arrow ⇐ if the code is recommended by Novitas for return trips
- A two-way single arrow ↔ if the code is in the non-Novitas list for outbound and return trips
- A right single arrow → if the code is in the non-Novitas list for outbound trips
- A left single arrow ← if the code is in the non-Novitas list for return trips
Add-on codes
Once a code is selected or typed in, AngelTrack consults its internal lists to see whether the chosen code has any recommended add-on codes. If there are any, the add-on code dropdown box lights up, offering the choices.
Although the Coding page UI displays the add-on codes in a different column than the primary codes, they are all submitted together when the claim is filed (or when an 837P is exported).
Reviewing the codes from previous dispatches
As a rule, each dispatch should be coded independently from all other dispatches... even from prior calls for the same patient to the same destination. The biller should choose codes organically, based on the narrative and other data in the run report.
That's the goal, anyway. To that end, AngelTrack does not offer any UI buttons to automatically copy the codes from the patient's prior trip. You can, however, switch to the "History" tab to review the codes used for the patient's prior calls, for the purpose of familiarizing oneself with the code titles and categories applicable to the patient.
Input from crews and QA
The PCR collects high-level (mostly .XXX) codes from the attending, representing the attending's impression of the patient, the patient's acute symptoms, and the causes of injury (if any). Although these are non-specific codes, they may serve as useful pointers when selecting the appropriately specific codes for the claim.
The PCR's code selections are displayed in the run report. To learn more about the PCR's code selections, read the ICD-10 Codes in the PCR guide.
The Significance of the First and Second Diagnosis Codes
Guidance from Novitas -- the premier MAC -- directs EMS billers to use the first diagnosis code to justify the transport and the second diagnosis code to justify the stretcher. Additional codes can be added to further justify either the transport or the stretcher.
For the secondary diagnosis code (the stretcher justification), for dates of service prior to 2023-02-09, Novitas LCD L35162 provided a list of just five preferred codes to choose from. The five codes are built into AngelTrack and always appear in the dropdown list for the second diagnosis code:
- Z74.01: Bed confined (must meet all three requirements)
- Z74.3: Need for continuous supervision by a care provider
- Z78.1: Need for physical restraints
- Z99.89: Need for enabling machines and devices
- Z76.89: No need for ambulance service (also use GY modifier)
For dates of service on or after 2023-Feb-09, after the end of LCD L35162, AngelTrack defaults the secondary diagnosis code box to "Other", so that you can choose a diagnosis code normally.
Automatic rearrangement of codes when necessary
If you specify an add-on code for the primary code, then the addon will be placed after this special secondary code in any 837P or CMS-1500 that AngelTrack generates for you in order to meet MAC expectations. For example, if you code your call like this:
| Diagnosis Code | Add-on Code | |
|---|---|---|
| Primary | S02.01XA | S06.890A |
| Secondary | Z74.3 | [Not applicable] |
| Tertiary | S03.1XXA | [None] |
...then AngelTrack will emit a claim with the following diagnosis codes: S02.01XA, Z74.3, S06.890A, and S03.1XXA, ensuring that the secondary code is always in the second slot where the MACs expect it to be.
Upcoding and Downcoding
AngelTrack will automatically select a procedure code based on:
- Service level requested
- Dispatch priority
- Crew Enroute driving (emergent/non-emergent)
- Crew transport driving
- QA review determination of service level performed
- Vehicle type
The auto-selected procedure code will be underlined like this:
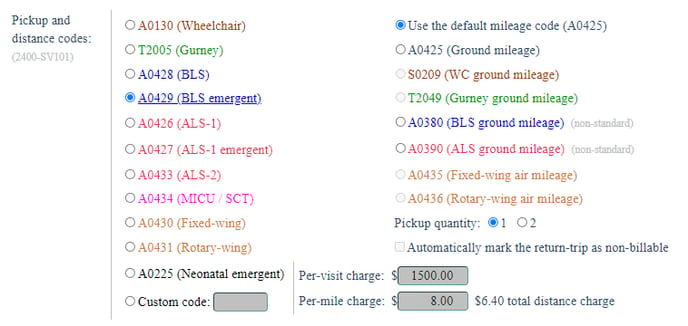
You can override the auto-selected procedure code by clicking any of the other choices. Your override will then be emitted in any insurance claims your issue and will likewise be honored by the invoice generators later in the billing process.
However, before you perform an override, have a talk with your QA reviewer first. A high-function organization will produce agreement between the QA reviewers and the billers. If they disagree about a call, then they should meet and discuss until they resolve their differences. The resolution can then be expressed in a new policy document that is disseminated to both departments (perhaps using an AngelTrack announcement).
Procedure HCPCS code auto-selection concerns
The auto-selected procedure code depends on the factors listed above, but in any case is capped by the determination made during QA review.
For example, if the QA reviewer determines that BLS service was provided, then the Coding page and the invoice generators will auto-select A0428 or A0429 (depending on whether the trip was emergent); they cannot auto-select any higher HCPCS codes like ALS or MICU because that would violate the determination made in QA.
This is true even if the dispatch was originally requested for a higher service level. For example, a call booked for MICU service but QA reviewed as BLS will always be treated as BLS throughout the billing process.
Furthermore the QA Review page requires the reviewer to affirmatively select what service level was provided. AngelTrack analyzes PCR data to make a suggestion, but the suggestion is not auto-saved; the reviewer must always click to confirm it. Therefore the only way that an inappropriately high service level could be auto-selected during coding or invoicing is if someone jumps the dispatch over QA review... a practice that should be forbidden except in special cases and with great caution.
Nonstandard HCPCS codes for pickup and mileage
Some state Medicaid carriers use nonstandard procedure codes for pickup and/or for mileage. You can enter a nonstandard procedure code for the pickup, and you can select one of the alternative mileage codes according to the requirements of the carrier.
If you choose a nonstandard procedure code for the mileage, then AngelTrack will match up the code with the appropriate price schedule in your retail price schema (or in the patient schema you selected) to determine the per-mile price.
If your Medicaid carrier wants you to claim a non-standard pickup code and no mileage code, for example you might be asked to claim A0140 for car service up to 16 miles, then you can input $0.00 in the field for per-mile charge, and then AngelTrack will omit any claim for mileage.
Nonstandard pickup codes are not honored by the invoice generators
AngelTrack's invoice generators do not honor any custom (i.e. non-standard) procedure code set during coding; in that situation, the invoice generators will invoice for the service that was determined by the QA reviewer.
Pickup Quantity
You can optionally set the pickup quantity to 2, instead of 1, if the carrier requires you to file a single claim for a special round-trip transfer, such as a wait-and-return.
Before using this option, review the Round Trip Claims Guide.
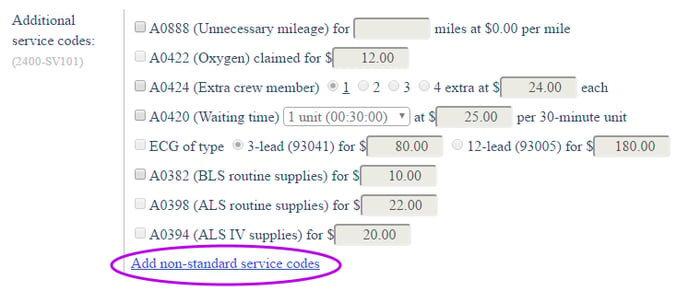
☑ A0422 (Oxygen)
AngelTrack will enable the ☑ A0422 (Oxygen) checkbox when the crew says (via a PCR medication record) they gave oxygen to the patient. However, AngelTrack will not automatically tick the box to claim it; the biller must choose to do so.
When the A0422 box is checked, then a price must be input. If you have configured a price for A0422 line items using the Pricing page, it will be pre-loaded into the field.
The quantity of oxygen is always one unit; therefore you are not required to specify the quantity.
Medicare does not pay for A0422 service lines, but secondary insurers sometimes do, so AngelTrack will automatically add the GY modifier to any A0422 service line being filed against a Medicare primary insurer. The MAC will remove the modifier when forwarding the claim to the secondary. See this CMS bulletin and also this one for details. If you do not want AngelTrack to automatically add the GY modifier in this situation, you can disable it under Settings | Preferences | "Billing".
☑ A0424 (Extra Crew Member)
AngelTrack will enable the ☑ A0424 (Extra crew member) checkbox when the dispatch records show that more than two crew members (or more than one for a wheelchair/car call) were involved in the transport. It will also underline the number of extra crew members shown in the dispatch records so that you do not have to look it up.
Because AngelTrack does not know whether the extra crew members were medically necessary, it will not automatically tick the checkbox to claim them. The biller must choose to do so after reviewing the narrative.
When the A0424 box is checked, then a price must be input. If you have configured a price for A0424 line items using the Pricing page, then that price will already be filled in for you.
Medicare does not pay for A0424 service lines, but secondary insurers sometimes do, so AngelTrack will automatically add the GY modifier to any A0424 service line being filed against a Medicare primary insurer. The MAC will remove the modifier when forwarding the claim to the secondary. A fuller explanation is given in the linked CMS bulletins just above. If you do not want AngelTrack to automatically add the GY modifier in this situation, you can disable it under Settings | Preferences | "Billing".
☑ A0420 (Waiting Time)
AngelTrack will enable the ☑ A0420 (Waiting time) checkbox when the dispatch records show that at least 30 minutes was spent waiting on the scene and/or at the destination. It will also pre-select the appropriate number of 30-minute units so that you do not have to look it up.
Because so few carriers cover this service, AngelTrack does not automatically tick the checkbox to claim it. The biller must do so after verifying that the carrier will pay it.
When the A0420 box is checked, then a price must be input. If you have configured a price for A0420 line items using the Pricing page, then that price will already be filled in for you.
Medicare does not pay for A0420 service lines, but a few secondary insurers sometimes do, so AngelTrack will automatically add the GY modifier to any A0420 service line being filed against a Medicare primary insurer. The MAC will remove the modifier when forwarding the claim to the secondary. A fuller explanation is given in the linked CMS bulletins just above. If you do not want AngelTrack to automatically add the GY modifier in this situation, you can disable it under Settings | Preferences | "Billing".
T2007 (Non-emergency waiting time)
T2007 is an alternative way to bill for waiting time. Probably you would only use it for gurney-van and wheelchair trips, unless your state Medicaid office specifically requests that you use it for BLS/ALS services.
In any case, AngelTrack's Coding page does not automate this HCPCS code, so you must use the "Add non-standard service codes" feature to claim it, discussed further below.
For the quantity claimed, the standard says they are in 30-minute units, but your state Medicaid office may require something different.
☑ ECG (93041 or 93005)
AngelTrack will enable the ☑ ECG checkbox when the crew says (via the PCR data) they administered an ECG to the patient. However, AngelTrack will not automatically tick the box to claim it; the biller must choose to do so.
When the ECG box is checked, then the type of ECG must be selected: if it has twelve or more leads, the procedure code is 93005; otherwise, the procedure code is 93041. A price must also be input. If you have configured a price for 93041 and 93005 line items using the Pricing page, then the prices will already be filled in for you.
Medicare does not pay for ECG service lines, but secondary insurers sometimes do, so AngelTrack will automatically add the GY modifier to any ECG service line being filed against a Medicare primary insurer. The MAC will remove the modifier when forwarding the claim to the secondary. A fuller explanation is given in the linked CMS bulletins just above. If you do not want AngelTrack to automatically add the GY modifier in this situation, you can disable it under Settings | Preferences | "Billing".
☑ DMS (A0382 or A0398)
A few insurance carriers will pay for Disposable Medical Supplies [DMS] claims that accompany an ambulance transport claim.
AngelTrack will enable the ☑ A0382 checkbox whenever a BLS or higher transport has occurred; likewise, it will enable the ☑ A0398 checkbox whenever an ALS or MICU transport has occurred. However, AngelTrack will not automatically tick the checkboxes to claim them; the biller must choose to do so.
If claimed, then a price must also be input. If you have configured a price for A0382 and A0398 line items using the Pricing page, then the prices will already be filled in for you.
Medicare does not pay for ambulance supplies service lines, but secondary insurers sometimes do, so AngelTrack will automatically add the GY modifier to any ambulance supplies service line being filed against a Medicare primary insurer. The MAC will remove the modifier when forwarding the claim to the secondary. A fuller explanation is given in the linked CMS bulletins just above. If you do not want AngelTrack to automatically add the GY modifier in this situation, you can disable it under Settings | Preferences | "Billing".
☑ A0394 (IV Supplies)
AngelTrack will enable the ☑ A0394 checkbox when the crew says (via the PCR data) that they installed, maintained, or removed an IV. However, AngelTrack will not automatically tick the box to claim it; the biller must choose to do so.
When the IV supplies box is checked, then a price must also be input. If you have configured a price for A0394 line items using the Pricing page, then the price will already be filled in for you.
Medicare does not pay for IV supplies service lines, but secondary insurers sometimes do, so AngelTrack will automatically add the GY modifier to any IV supplies service line being filed against a Medicare primary insurer. The MAC will remove the modifier when forwarding the claim to the secondary. A fuller explanation is given in the linked CMS bulletins just above. If you do not want AngelTrack to automatically add the GY modifier in this situation, you can disable it under Settings | Preferences | "Billing".
Non-Standard Service Lines
A few commercial carriers will pay for unusual procedure codes when submitted as additional service lines in the claim. For example, an EMS company may be permitted to claim (via an additional service line) a small charge for each medication that was administered.
Such claims are made using whichever codes the carrier dictates, in its policy documentation or in its 837P companion guide. To add one of these non-standard procedure codes to your claim in AngelTrack, click "Add non-standard service codes":
AngelTrack will then display a grid of the non-standard service codes already present in the claim. The grid will be empty at first; click the ![]() icon to add one, fill out the popover form, and then click "Save".
icon to add one, fill out the popover form, and then click "Save".
You must specify all modifiers for each service code, with the exception of the ET modifier (which always comes first when present) and the location modifier (which always comes next). Both are handled automatically by AngelTrack.
No guarantees and no technical support is offered for non-standard service lines
It is your responsibility to understand the carrier's offer to pay on non-standard codes and to correctly input the codes and modifiers and notes. You must also consider the effects on the secondary carrier (if any). AngelTrack does not attempt to satisfy every carrier's idiosyncrasies, and so if AngelTrack is unable to produce an electronic claim with the desired non-standard elements, then you must resort to paper claims instead and modify them yourself.
Do not call AngelTrack Support for help with non-standard codes and carrier requirements.
Location Modifier / Ambulance Modifier
In a claim for EMS services, the first modifier after the service code is called the "ambulance modifier" or "location modifier". Here is a service line from an EMS claim showing the location modifier in its proper position at the head of the list of modifiers:
LX*1
SV1*HC:A0428:RJ:GY*1500*UN*1***1:2
DTP*472*D8*20150601
REF*6R*AS3N1
A location modifier is made from two individual HCPCS location codes, one for the origin and one for the destination. To learn more about location modifiers and how AngelTrack automates them, read the Location Modifiers Guide.
☑ GM Modifier
The GM modifier is used to inform the carrier that the ambulance was simultaneously transporting more than one patient. The carrier will then pay a moderately reduced rate for each transport.
AngeTrack will automatically select the GM modifier if the dispatch records show that this call's transport time overlapped another call's transport time in the same vehicle.
Consequently, AngelTrack may erroneously tick the GM checkbox if your dispatch records are incorrect. Remember, the crew -- or, failing that, the dispatcher -- is responsible for marking the time transport began and the time arrived at the destination. If either mark was missed or incorrect, the attending or the dispatcher must edit the follow-up information to set it right. If they fail to do so, then the transport timeframe might overlap the timeframe of the vehicle's previous or next transport.
So, if AngelTrack is incorrectly ticking the GM checkbox, send the call back to QA with a billing note. Or you can open the run ticket, visit the follow-up page, and correct the times yourself. To identify the overlapping call, use the "Vehicle's prior call" and "Vehicle's next call" links that appear next to the odometer readings near the top of the Dispatch Followup page.
☑ GY Modifier
You are probably already familiar with the GY modifier, which is used to signal the carrier that you understand this claim will be denied. When the ☑ GY checkbox is ticked, AngelTrack will add the "GY" modifier to the claim. Do not include GY or any other special modifiers in the "Location Modifier" textbox.
The ☑ GY checkbox will be automatically ticked for you if the patient signed a "Non-Covered Destination / Advanced Beneficiary Notification" document for the dispatch in question... but of course, you can untick it as you see fit.
Automatic GY modifiers for Medicare claims
Medicare does not pay for oxygen (A0422), for extra attendants (A0424), or any of the DMS codes, but secondary insurers often do. Medicare MACs support the use of the GY modifier only on those uncovered service lines; the MACs will then forward the claims to the secondary carrier with the GY modifier removed. See this CMS bulletin and also this one for details.
In anticipation of this, AngelTrack will automatically add the GY modifier to all secondary service lines (i.e. everything other than the pickup code and the mileage code) when the claim is bound for Medicare as the primary insurer. If you do not want AngelTrack to automatically add the GY modifier in this situation, you can disable it under Settings | Preferences | "Billing".
Do not tick the ☑ GY checkbox unless you want the modifier applied to the entire claim.
☑ QL Modifier
This modifier is used to signify that the patient died after the ambulance was called but before the ambulance arrived. EMS arrives on the scene and simply confirms the patient's death.
EMS is entitled to reimbursement for the pickup, but obviously not for mileage. See section 10.2.6 "Effect of Beneficiary Death on Medicare Payment for Ground" of the Medicare Benefit Policy Manual chapter 10.
If the QL modifier is selected, then AngelTrack automatically applies it to all service lines in the claim.
The carrier may not want a location modifier in this situation. To accommodate this, AngelTrack allows the location modifier to be blank when ☑ QL is ticked.
☑ QJ Modifier
This modifier is used to signify that the patient is incarcerated yet is responsible for paying their own medical bills. In other words, the patient is incarcerated yet the state or local government does not pay for their healthcare.
If the QJ modifier is selected, then AngelTrack automatically applies it to all service lines in the claim.
☑ CR Modifier
This modifier is used to signify that the services provided were related to a catastrophe. AngelTrack will automatically pre-select this modifier if the crew specifies any catastrophe-related injury causes in the PCR Injury form.
If the CR modifier is selected, then AngelTrack automatically applies it to all service lines in the claim.
☑ 76 Modifier
This modifier is used to signify that the services provided were a repeat of the same services already provided earlier on the same day. This is not for use on a return trip for an outbound trip, rather it is for claiming a second outbound trip that duplicates an identical outbound trip earlier the same day, such as a second trip to an ER after first returning to the nursing home.
Using its dispatch records, AngelTrack may automatically select the 76 modifier for you, but this can be overridden.
If the 76 modifier is selected, then AngelTrack automatically applies it to all service lines in the claim.
Nonstandard Modifiers
State Medicaid carriers often require nonstandard procedure codes, non-standard modifiers, and nonstandard modifier orders. AngelTrack supports most of these practices. However, you should not use any of these modifiers unless you are certain that the carrier requires it!
☑ ET Modifier
The ET modifier is an obsolete method of flagging the transport as emergent. If you check the box, then the ET modifier will appear first in the list of modifiers for the call, in front of all other modifiers including the ambulance modifier.
Only a few insurers still accept/require the ET modifier. Do not check the box unless you know that the carrier specifically requires it.
The ☑ ET checkbox will be disabled (greyed out) if the underlying dispatch was not actually emergent. If you believe it should've been marked emergent, send it back to QA for re-review.
☑ QN Modifier
This modifier is normally used only by a hospital that operates its own ambulance service. That ambulance division will specify QN to explain why it did not file for prior authorization.
Normally this situation would never come up for a standalone EMS operation, but certain state Medicaid carriers require this modifier and interpret it differently; they use it in place of QM, which means that ambulance transport was arranged by the facility rather than furnished by the facility. For this situation, AngelTrack makes the QN modifier available for use.
☑ UB Modifier
Some state Medicaid carriers accept the UB modifier, which is used to indicate that transport mileage was not emergent. The carrier's 837P Companion Guide will say whether they accept this modifier.
☑ UJ Modifier
Some state Medicaid carriers accept the UJ modifier, which is used to charge a little extra for ambulance service that was provided between 19:00 at night and 07:00 the next morning. The carrier's 837P Companion Guide will say whether they accept this modifier.
The ☑ UJ checkbox will be disabled unless the transport time at least partially overlaps the time period of 19:00 to 07:00.
☑ 32 Modifier
Some state Medicaid carriers accept the 32 modifier, which requests special consideration for a claim that normally would require a PAN but there was no time to get one, similar to how emergent trips do not require a PAN.
☑ Q4 Modifier
Some state Medicaid carriers accept the Q4 modifier, which requests coverage without a PAN for a discharge or interfacility transport.
☑ QM Modifier
The QM modifier is used to indicate that transportation was provided under a prearranged contract, such as that for a prison.
☑ U1, U2, U3, U4, U5, and U6 Modifiers
These modifiers are used by some state Medicaid carriers in situations where you are claiming multiple near-identical trips for the same patient and same date of service. Select the one that indicates the ordinal number of the claim you are filing among all the trips taken that day by the patient.
Other nonstandard requirements
For nonstandard requirements beyond these, you must emit your claims as CMS-1500 forms and then perform the necessary touch-ups by hand.
The CMS-1500 emitted by AngelTrack has freely editable fields, which you can edit right in your browser. Of course, AngelTrack will fill in as many as it can, and then you can add or change values to suit your Medicaid carrier.
Treatment in Place / Catch and Release
You can file claims for treatment-in-place, catch-and-release, and related refusals, using the ET3-style claim format.
To learn how, visit the Treat and Release Claims Guide.
Reason for Transport / Reason for Stretcher
The "Reason for transport" and "Reason for stretcher" fields are initially populated by an algorithm in AngelTrack's database. The algorithm attempts to summarize the fields and data input by the crews (in the Followup) and then checked and revised during QA review. If the fields do not contain good starting data, then consider pushing the call back to QA for revisions.
Once the fields contain enough information, you must condense them to fit within the 80 characters allowed by the X12.837-P specification. The Coding page will indicate how many characters you've got in each field.
Incidentally, when filing CMS-1500 paper claims, the "Reason for transport" is omitted because there is no available box on the form. The "Reason for stretcher" is placed in box 19 ("ADDITIONAL CLAIM INFORMATION").
Ambulance Certifications / Loop 2300*CRC
Ambulance certification codes are the reasons why the patient required the care of EMS, as opposed to traveling by private car. The codes are submitted in loop 2300 CRC03, CRC04, CRC05, and so on.
The first time you code a claim, AngelTrack calculates which certification codes seem to be implied by the data in the dispatch record and PCR records; it then automatically ticks the relevant checkboxes for you. Once you click "Save", your selected checkboxes are preserved and will not be automatically re-ticked or un-ticked on subsequent visits to the Coding page.
If AngelTrack does not tick the checkboxes you expect, then there is probably something missing from the dispatch's documentation. Although you are free to tick additional boxes, you should probably send the dispatch back to QA instead, with instructions in the "Billing notes" field. That way your documentation will be safely complete in the event of an audit.
Most carriers want two or three certifications to be checked; one is usually too few, and four is usually too many.
If filing CMS-1500 paper claims, there is no box for ambulance certifications, so they will be omitted.
"Related Cause" / Accident Information / Loop 2300*CLM11
AngelTrack will automatically include accident information (loop 2300 CLM11) if the crew's run report indicates that an accident was the cause of injury.
There are four categories of related causes in an X12.837P claim. AngelTrack infers the correct category using the information provided by the crew in the PCR Injury form:
| PCR Injury Inferred Cause | X12.837P CLM11 | CMS-1500 Box 10 |
|---|---|---|
| Automotive accident | AA + two-letter state code of the dispatch's origin address |
☑ AUTO ACCIDENT? plus two-letter state code |
| Employment | EM | ☑ EMPLOYMENT? |
| Other accident | OA | ☑ OTHER ACCIDENT? |
| Another person | AP | [Not applicable] |
Specifically, AngelTrack looks at the ICD-10 code selected by the crew in the first (#1) "Causes" field of the PCR Injury form, plus the crew's answer to the ☑ The primary cause of injury is related to the patient's employment checkbox.
When a related cause is given in an insurance claim, then the date of occurrence must also be given (this does not apply to CMS-1500). AngelTrack will calculate this date using the information provided by the crew in the PCR Assessment tab's "Primary complaint duration" field. The date will be emitted in the X12.837P document in a DTP*439 segment, as described in the next section.
Event Dates
There are many event date fields in an X12.837P for an EMS claim, which AngelTrack automatically populates like this:
| Segment | Loop | Meaning in X12 Specification | Source of Data in AngelTrack | When Included in X12.837P by AngelTrack |
|---|---|---|---|---|
| DMG*D8 | 2010BA | Subscriber's date of birth | Patient Billing: Policyholder Date of Birth, or Patient Demographics: Date of Birth | When the policyholder's DOB is on file |
| DMG*D8 | 2010CA | Patient's date of birth | Patient Demographics: Date of Birth | When the patient's DOB is on file, and the patient is not the policyholder. |
| DTP*431 | 2300 | When did symptoms onset? | PCR Assessment: Primary Complaint Duration subtracted from the Date/Time Assessed | When an assessment has been performed that specifies a Primary Complaint Duration, if such date is different from the date of service (DTP*454), or when a date is manually specified on the Coding page |
| DTP*439 | 2300 | When did the accident occur? | PCR Assessment: Primary Complaint Duration subtracted from the Date/Time Assessed | When the PCR Injury: Primary Cause of Injury specifies an ICD-10 that is accidental, or when a date is manually specified on the Coding page |
| DTP*454 | 2300 | When did the provider treat the patient? | Followup: Date/Time Transport Began if available, else Dispatch: Date/Time Activated | Always |
| DTP*472 | 2400 | When was service rendered? | Followup: Date/Time Transport Began if available, else Dispatch: Date/Time Activated | Always |
| DTP*435 | 2300 | When was the patient admitted to a hospital? | PCR Hospital: Date/Time Admitted | When the PCR Hospital: Date/Time Admitted field is populated, or when a date is manually specified on the Coding page |
| DTP*096 | 2300 | When was the patient discharged from a hospital? | [This data is not collected in the PCR.] | When a date is manually specified on the Coding page |
| DTP*573 | 2430 | When was the primary claim adjudicated? | Date/Time of primary insurer adjudication, as reported in an X12.835 document | When claiming against a secondary after the primary has returned an adjudication |
You can review all these segments by loading the dispatch into the X12.837P Workbench, which is available from a link on the Coding page.
Overriding the event dates
The event dates for the onset of symptoms (DTP*431), for the occurrence of the accident (DTP*439), for admission to a hospital (DTP*435), and for discharge from a hospital (DTP*096), can be overridden from the values automatically populated by the PCR data.
If the PCR has no data for the onset of symptoms or occurrence of accident or admission to a hospital, the respective fields will be empty on the Coding page. You can manually input these dates if you wish; however, it is better to send the report back to the crew and ask them to provide the necessary date information.
Round Trips are Filed as Separate Claims
AngelTrack always files round trips as two separate claims in order to avoid the hazards of round-trip claims:
- The returned EOB will be marked "Approval" even if the return-trip leg is denied. It is therefore easy to misread the EOB, incorrectly concluding that both trips were approved.
- If one trip is approved but the other denied, it is a hassle to untangle and appeal or refile just the one trip.
- Commingled benefit lines on EOBs make it difficult for AngelTrack to achieve one of its design goals: simplified, accessible billing usable even by novices.
- The usual reason for combining trips in a round-trip claim is to minimize the amount of keyboarding and data entry, which is necessary when using traditional billing software that knows nothing of EMS and does not have access to your dispatch records. This reason no longer applies since AngelTrack pre-fills 90% of the claim with dispatch and PCR data.
Paperwork / Upload of Run Reports / Loop 2300*PWK
If a carrier requires you to upload a PDF of the run report for your claim, here is how to do it:
- Login to the carrier's website and find their paperwork-uploader page.
- From the Coding page in AngelTrack, using the links on the right-hand side of the page, fetch the run report as a PDF.
- Upload the PDF to the carrier's website. They will issue you a paperwork ID number.
- At the bottom of the Coding page in AngelTrack, find the "Paperwork" section at the very bottom, and input the paperwork ID number the carrier gave you.
- Save the Coding and then batch your claim.
The key insight here is that you must upload the paperwork in advance, before you transmit your claim.
ET3 Program
AngelTrack fully supports the billing and data-reporting requirements of the ET3 program, though it is now defunct.
To learn about ET3 claims, refer to the ET3 Integration Guide.
Dealing with Non-Compliant Carriers
Normally it is the job of your clearinghouse to scrub your claims to please each carrier's odd requirements. However, the clearinghouse's claim scrubber is limited: it cannot add new data fields where none existed before. For carriers imposing such requirements, AngelTrack can customize its X12.837P documents as needed.
Alternate provider ID required in loop 2310B REF02
A few insurance carriers require an alternate ID to be sent in loop 2310B element REF02, sometimes referred to as CMS-1500 box 24j. AngelTrack supports this request.
To learn how to do it, read the Alternate Provider IDs in REF02 Guide.
Alternate provider ID required in loops 2010AA REF02 or 2010BB REF02
Some Medicaid carriers issue alternate IDs and then require them to be submitted in a nonstandard loop in the X12.837P document. AngelTrack supports this request.
Open the Insurance Payor ID List and find the carrier's record. Open the record for editing and tick the appropriate checkbox:
- ☑ Requires the alternate provider ID in loop 2010AA REF02 - Tick this box if the carrier has assigned you a provider ID and requires you to send that ID back to them in loop 2010AA (Billing provider) element REF02.
- ☑ Requires the alternate provider ID in loop 2010BB REF02 - Tick this box if the carrier has assigned you a provider ID and requires you to send that ID back to them in loop 2010BB (Primary insurance payor ID) element REF02.
To take advantage of this workaround, you must configure the alternate ID (issued by the carrier) as instructed just above, and your biller must select that alternate ID while coding the claim.
No decimal mileage
If the carrier fails to support decimal mileage, demanding only whole numbers of miles transported, AngelTrack can handle it automatically.
Open the Insurance Payor ID List and find the carrier's record. Open the record for editing and tick the ☑ Fails to support decimal mileage checkbox. AngelTrack will thereafter automatically round all mileage quantities to the nearest whole number; any mileage quantity less than zero will be rounded up to one.
Demand for a Rendering Provider NPI when same as Billing Provider NPI
If your clearinghouse says your claims are missing their rendering provider NPI, or says your claims are giving the wrong taxonomy qualifier, then you are probably a single organizational NPI provider, but your clearinghouse isn't compliant with the X12.5010 standard's rules for such providers.
For an explanation of this problem, read the Single NPI Billing Guide.
Demand for no NPI in 2010AA/2310B
Some state Medicaid carriers require an 837P which completely omits the provider NPI(s). If you face this demand, and if your clearinghouse is willing to accept an 837P that is missing its provider NPI(s), AngelTrack can satisfy the demand.
Simply visit the Insurance Payor ID List, find the carrier in question, and tick the ☑ Requires a blank NPI element in loop 2010AA/2310B checkbox under "Compliance".
Demand for a custom ID number in Loop 1000A NM109
If a carrier requires a custom sender ID or provider ID in loop 1000A element NM109, different from your normal clearinghouse sender ID, you may configure one.
Simply visit the Insurance Payor ID List, find the carrier in question, and fill out the field named "Requires a custom ID in loop 1000A element NM109" under "Compliance". Afterward, all claims bound for the selected carrier will be automatically separated into their own batch, as they cannot be intermingled with other claims that use a standard loop 1000A.
Special CMS-1500 markup
For each carrier in the Insurance Payor ID List, you can specify additional customizations to AngelTrack's CMS-1500 markup to meet the carrier's special requirements.
Whenever AngelTrack emits a 1500 claim against that carrier, those customizations will apply. To learn more, refer to the Insurance Payor ID List Guide.
Next Steps
Once the coding is finished, click "Save" and return to the Insurance Filing Queue.
If not using AngelTrack's uploader to transmit the call to a clearinghouse, you can then export your work as a completed X12.837P document, suitable for upload to a clearinghouse of your choice (or directly to your MAC). This document is sometimes called an X-12 file; you can download it right from the Insurance Filing Queue.
To learn more about transmitting your claims to your clearinghouse, read the Filing a Coded Claim guide. To learn more about managing your 837P batches of claims, read the Batch Management guide.
Coding and Price Quotes
The many settings and charges on the Coding page do not directly control the dispatch's price quote and thus do not directly alter its balance due. Rather, the Coding page controls the total price that will be claimed.
AngelTrack will not update the price quote to match the Coding page until you create a new claim batch and then mark it Transmitted.
This is part of AngelTrack's system of "lazy price quoting" and is further discussed in the Pricing and Price Quotes Guide.